DIGITAL DEFORMITY: SURGICAL INTERVENTION THROUGH AN ARTHROPLASTY OF THE PROXIMAL PHALANX.
The digital deformity of the smaller toes is every time, a pathology of greater surgical demand in the podologic centers and it must not be considered as a minor problem, because pain and deformity may have a significant impact in the patient’s quality of life. In the middle of the twentieth century, it was registered with an incidence of 20 % among the population according to Mann, with no significant differences between sexes, keeping in current surveys with an incidence of 20 %, but there are frequently more cases in women and at older ages. These data aren’t indifferent to us because they verify the existence of this deformity. Therefore, it can not be considered less important in connection with other osteoarticular pathologies of the foot, reaffirming the need of making a good surgical intervention, considering the patient’s needs bearing in mind the indications and contraindications of suitable techniques, for a correct praxis.
There is a certain misinterpretation in the nomenclature of the deformities of the smaller toes generalizing by the name of “claw deformitites “ according to Schrier and Associates. The claw toes, strictly speaking, affect to the metatarsophalangeal joint, proximal interphalangeal and the distal interphalangeal joint. It is important to emphasize that there is a subclassification (Coughlin, MG) regarding the claw deformity, which include: the claw toe, hammer toe and mallet toe, although the remaining deformities probably are part of the same pathologic process, so they will be treated in a similar way.
The hammer toes are defined as the proximal interphalangeal flexion with or without participation of the distal interphalangeal joint, while the claw toes are defined as the extension of the metatarsophalangeal joint, jointly with the flexion of the proximal interphalangeal joint and the distal interphalangeal joint. Besides, these last ones frequently are associated with neuromuscular alterations and generally imply a bilateral condition without affecting the toes; in contrast to the hammer toes which they use to be produced in an isolated way, being the second toe the most commonly affected (Canale ST). A third classification describes mallet toes, these are less common than hammer toes (ratio 1: 9) (Hetherington VP). The deformity frequents that a toe will be longer than the adjacent toes but it is produced with the same frequency in the second, third and fourth toe being called as the flexion of the distal interphalangeal joint without any alteration of the interphalangeal and the metatarsophalangeal joint.
Speaking in a physiopathologic way, there is a big relationship between the deformity and the anatomical patterns (mainly myotendinous), coming up in this way three pathomechanical models of the digital deformity which show the possible muscular imbalances: model of flexor extensor replacement and flexor stabilization. At the same time, the importance which has the role of the intrinsic muscles during the stabilization of toes when the roaming takes place. This fact has brought to different authors like Hetherington to distinguish the digital deformities in two kinds: in static and dynamic.
The model of flexor stabilization takes place when exists a mechanical advantage of the toe’s common long flexor and/or the toe’s common short flexor above the interosseals in the period of the medium support of walking. Therefore, the interosseals are not able to stabilize the toe. (Root et al). They observed that a pronated foot caused that the plantar square would lose its mechanical advantage, not tractioning sideways the flexor apparatus, which causes a claw and the varus rotation of the fourth and fifth toe. The model of flexor replacement is produced when there is a dysfunction or debility of the sural triceps. It is the less common of the three. This early and continuous activity causes that the flexor group gets easily a mechanical advantage over the interosseal muscles, forming in this way, the toe’s contraction, which will be obvious in the final period of the middle support and the beginning of the propulsive period.
These considerations are very important when we decide to make a procedure about the soft tissues. This makes that making tenotomies of the extensors have little sense when the flexor stabilization or the flexor replacement is the primary cause of the deformity of the toes. The pattern of extensor replacement, takes place when the common long extensor of toes gets mechanical advantage on the lumbrical and interosseal muscles in the walking wobble phase. Sarrafian and Topouzian describe the great importance of the extensor apparatus in the digital deformities by the designated “Extensor wing mechanism” and “The sling mechanism of extension”. Passively, flexor tendines will make a plantar flexion of the interphalangeal joints, together with an increase of the subtalar pronation, producing a clear abduction of the front part of the foot. With these kind of conditions the plantar square loses its lateral vector making only strength in a proximal direction. With the abduction of the front part of the foot, the plantar square is not able to correct the medial obliquity of the toe’s long flexor tendo. This can also be caused by an inappropriate dorsiflexion of the ankle as a result of a short Achilles tendon or an osseous anomaly which allows an echino ankle or by the existence of weak lumbrical muscles or the spasticity of the long extensor of the toes. To understand the pathomechanics of these deformity patterns will be of vital importance in surgical operations on soft tissues.
Many of these deformities will be treated successfully with conservative methods, but depending on the seriousness of the deformity and if this is fixed or flexible, through a previous clinical examination with different evaluative proceedings and reducibility tests (Kelikian AS), we can find a series of possible surgical options ir order to solve the problem. Its correction can be achieved using a progressive method of the soft tissues proceedings, osseous proceedings or a combination of both.
In the clinical case, it is set out the case of an impregnable hammer toe with affectation of the proximal interphalangeal joint and retraction of soft parts. It will be made by a longitudinal intervention, an arthroplasty from the head of the proximal phalanx by the hammer technique and a temporal intramedullary Kishner needle implantation. It will also be assessed the pre-surgical and post-surgical pain by the AOFAS pain scale and a monitoring will be made if there are possible complications in three months.
C L I N I C A L C A S E
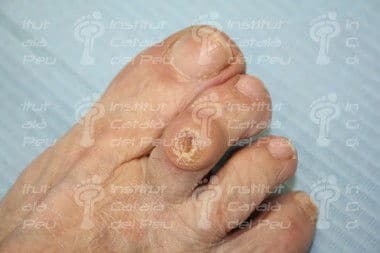
83 year old patient with algia at a second metatarsal head level, in a dorsal and plantar way in the right foot (the pain lasts intermittently since five years ago, but it is stronger during the last 6 months). She shows previous cases of hypertension, hypercholesterolemia and osteoporosis, being her current medication the next ones: Enalepril 5 mg, Orfidal 1 mg, Netecal 600 mg, Adiro 100 mg and Zocor 20 mg. She has no well-known allergies and says that she has never had any orthopedic treatment. It is observed together with the clinical exploration a first radius with normal mobility and without pain signs while in the exploration of the second radius shows pain at the distoproximal and proximodistal pressure of the metatarsal head, at the direct pressure of the metatarsal head and the proximal interphalangeal joint, giving a positive sign in the Keliquian’s and Mulder’s test, therefore AMTF is not luxated. It is not perceived a limitation to the mobilization of the metatarsophalangeal joint of the second radius but it does to the mobilization in plantar flexion being its movement level in 0 stage both in a normal assessment and in a vertical stress. The metatarsal position regarding to the frontal view is assessed in plantar flexion. The proximal interphalangeal joint shows a limited mobility in dorsal flexure and plantar flexion, therefore irreducible and with a level in stage 3 in the vertical stress test while the distal interphalangeal joint shows a normal mobility.
When we palpated this proximal interphalangeal joint we noticed a dorsal osseous protuberance and the existence of a big dorsal heloma. At the same time, we could see the contracture of the common long extensor of toes.
In the radiological test, doctors made a dorsum plantar in charge projection to her and another lateral, where it could be seen the luxation of the proximal interphalangeal joint and a metatarsal formula of index minus. The patient was diagnosed as having irreducible hammer toe and doctors gave her the option of being operated on. The intervention technique was an arthroplasty with fixation by a Kirschner needle together with a tenotomy of long extensor of toes by MIS technique (minimum incision). The required documentation was done (rights of image, informed consent, analysis and radiographies) and they explained her the guidelines to follow before and after the intervention.
It was made to the patient a foot asepsis and surgery was being prepared. It was applied to her nerve block anesthesia with Mepivacaine 3 % at a level of the second toe infiltrating in the medial, lateral and dorsal branch at the level of the metatarsophalangeal joint and moreover, two boosters across from plantar- medial to dorsum-lateral and the other way around. She was given a dose of 0,9 cc altogether.
The intervention through the resection arthroplasty starts with an incision with a longitudinal overture being this one at the level of the interphalangeal joint with number 15 bistoury covering a big part of the proximal phalanx and the medium phalanx. The first incision was with the venter of the bistoury and the second one by touching with the point of the bistoury. The dissection was made by layers starting in the epidermis, the subcutaneous tissue and superficial fascia until it came to the deep fascia, using the mosquito tool in the medial side and the lateral side of the incision. Then we will cauterize the superficial blood vessels and afterwards we will cut off the ELCD tendon.
Once the articulation is free from adherences we make the capsulotomy of the articular capsule by a reversed L with a bistoury of 15º. Next step is to proceed to the section of the collateral ligaments which join the two phalanges in order to show the head of the proximal phalanx through a Mcglamery elevator. Then we wil make the resection of the head of the proximal phalanx by bone metal shears and we will proceed to its remodeling with Joseph’s lime to eliminate possible dorsal edges which could cause a postsurgical pain. Finally, the articulation is examined to check if it is properly located in a sagittal plane. When noticing a light retraction in the extension of one toe we will proceed to the tenotomy of the long extensor of the second toe.
After the resection of the articular surface, we put a Kischner needle through the medium and distal phalanx in order to immobilize the foot’s toe tip and then the Kischner needle is reverted to the proximal phalanx. We will check by a fluoroscopy the location of the Kischner needle. We will suture by layers in a tightening way by a reabsorbable thread of 5/0 in capsule and with 4/0 reabsorbable the subcutaneous tissue and we will suture skin by silk 3/0. It is applied a bandage with gauzes covering the interventioned toe and making an anterior arch for the appropriate fixing of the metatarsal formula.
When the intervention had finished it was given a Nolotil 575 mg to the patient and she was provided guidelines of pharmacologic therapy based on Ibuprofeno 600 mg every 8 hours during 7 days and if there is pain Nolotil 675 mg. It wasn’t made a postsurgical radiography to her. The postsurgical monitoring was done in the three following months after the surgery. After 48 hours of the first cure the bandage was removed and it were not detected any inflammation or infection signs with a proper process of cicatrization. She was applied some povidone-iodine and also some bandage. The pain scoring according to AOFAS scale was 36 points over 40, where there is a great improvement with regard to the presurgical where the results were in the second cure (7 following days) the suture points were removed and were applied approach to strip for preventioning. It had a good appearance and she was applied povidone-iodine and bandage.
In the third cure the K-needle was extracted. There hasn’t been a bad fusion of the bone nor instability.

Dorsum-plantar projection in charge. Watch the luxation of the proximal interphalangeal joint of second toe.

Nerve block anesthesia with Mepivacaine 3 % at the level of metatarsophalangeal joint of second toe. Medial branch.

Nerve block anesthesia with Mepivacaine 3 % at the level of metatarsophalangeal joint of the second toe. Dorsal branch.























Leave a Reply
Want to join the discussion?Feel free to contribute!